Disclaimer: This guide is educational and not a diagnosis. Treatments discussed may be off-label for Long Covid and are considered case by case.
Long COVID is not just “taking longer to get better.”
Unfortunately, for many people, COVID-19 infection can trigger persistent symptoms that last 3 months or longer post-infection. This comes in waves of troubling symptoms, which can include exhaustion, brain fog, dizziness, or chest tightness.
Unlike other illnesses, where you progressively feel better over time, long COVID’s symptoms don’t follow the typical path of recovery. Understanding why this happens is the first step toward effective treatment and resolution of symptoms.
Why Long COVID Doesn’t Behave Like a Normal Recovery
Normally, after a viral infection, the body heals over time. Post-COVID-19 condition represents a persistent biological state. The immune system, vascular system, and nervous system all remain dysregulated long after the virus has cleared, causing a troubling and debilitating cluster of symptoms.
This is why “rest and time” often fail. Instead of steady improvement, many patients experience relapse or flare cycles. They can feel well for one week, then suddenly struggle again after minor exertion. It’s a pattern seen in other chronic illnesses, such as chronic fatigue syndrome or autoimmune conditions, where inflammation and poor circulation keep the body in a loop.
Common effects include:
- Ongoing fatigue with cognitive slowdown and/or chest discomfort.
- Difficulty working or inability to sustain normal daily routines.
- A reaction to physical or emotional stress that feels disproportionate.
It is important to note that at its core, Long COVID is biological, not psychological.
The Core Biological Problem: Inflammation That Doesn’t Switch Off
Systemic and Vascular Inflammation.
During infections, inflammation ramps up as part of the immune response to fight the virus, then settles down once the virus clears, and the healing phase begins. In Long COVID, immune dysregulation means this switch-off mechanism fails, creating a state of chronic inflammation.
Traces of immune activation linger especially within your vascular system, which is the network of blood vessels that delivers oxygen and nutrients to every cell.
The endothelium, which is the layer of cells that lines these vessels, becomes irritated (a process called endothelial inflammation). Receiving a diagnosis is frustrating because blood tests may look “normal” as routine blood panels don’t detect microvascular distress or low-grade cytokine activity.
Key biological changes may include:
- Cytokine imbalance (the body’s inflammatory signalling proteins are high whilst anti-inflammatory signalling proteins are low).
- Endothelial irritation creates “stickier” vessel walls, which are also inflamed.
- Impaired microcirculation, micro-clots inhibit oxygen and nutrients from reaching tissues effectively.
Inflammation That Becomes Self-Sustaining
When the vascular system is inflamed, oxygen delivery begins to falter. This lack of oxygen worsens inflammation, creating hypoxia and forming a feedback loop.
When oxygen debt builds up, patients experience deeper fatigue, brain fog, and exercise intolerance, which is often described as post-exertional malaise (PEM).
This mechanism explains why pushing through symptoms or attempting “graded exercise therapy” can backfire. In fact, more activity can intensify inflammation rather than rebuild strength. Gentle pacing, on the other hand, helps to stabilise energy levels without triggering setbacks.
Symptoms linked to this often include:
- Fatigue that worsens rather than improves with rest.
- Chest pressure, shortness of breath, and heart rate spikes after minimal exertion.
- Cognitive or sensory overload following mental strain.
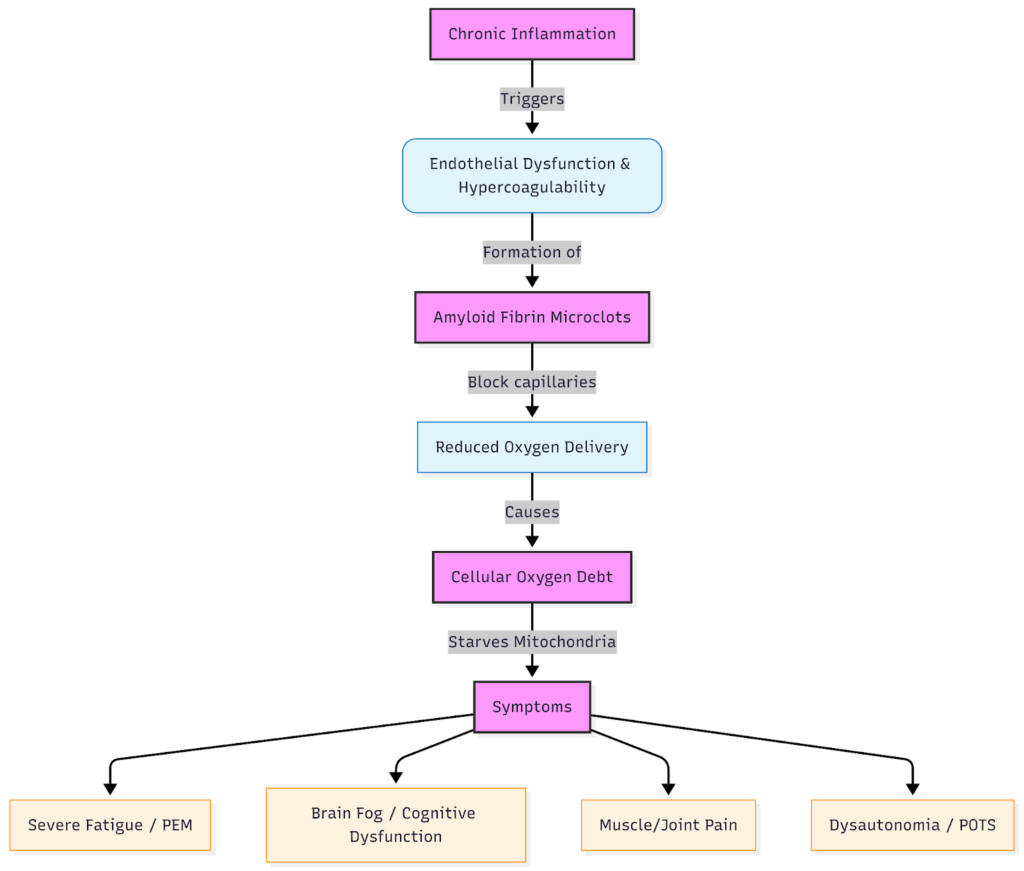
Microclots: How Blood Flow Gets Blocked at the Smallest Level
What Are Microclots?
One of the key biological findings in Long COVID is the presence of fibrin amyloid microclots, which are tiny, resilient clumps within the bloodstream. Unlike typical clots that can be seen with imaging, these microthromboses form at the microscopic level and evade routine tests.
They are linked to platelet hyperactivation, meaning the blood’s clotting cells stay unusually “sticky.” While this response may start as protective, prolonged microclot formation reduces oxygen delivery where it’s needed most.
How Microclots Reduce Oxygen Where It’s Needed Most
Capillaries are the smallest blood vessels in your body, and the average person has between 60,000 and 100,000km of them. Capillaries perform a very important role, and they are where oxygen passes from the blood to the tissue. Microclots from Long COVID can block these pathways, leading to tissue-level hypoxia or what patients often describe as “oxygen debt.”
This oxygen debt often won’t always show up on a pulse oximeter, because those devices measure oxygen in blood, not its delivery to cells. However, a venous blood gas analysis can sometimes indicate if there are issues with oxygen delivery.
The systems affected by microclots and your symptoms may include:
- Muscles → rapid exhaustion, heaviness, post-exercise crashes.
- Brain → poor concentration, memory lapses, “foggy” thinking.
- Autonomic system → dysautonomia symptoms like temperature swings or heart rate instability.
Oxygen Debt: Why Your Cells Are Running on Empty
Oxygen Delivery vs Oxygen Saturation
Your pulse oximeter may read 98%, yet your muscles and brain may still be struggling to receive oxygen. This gap between blood oxygen content and delivery defines the “oxygen debt” state seen in many Long COVID patients.
Why Exertion Makes Symptoms Worse
Exertion increases the body’s oxygen demand. When microclots and mitochondrial stress block supply, symptoms quickly escalate. This underlies post-exertional malaise (PEM) seen in both Long COVID and chronic fatigue-related conditions, where the body’s recovery systems simply can’t keep pace with energy use.
Nervous System Involvement
Autonomic Dysfunction (Dysautonomia) and POTS
A subset of patients develops a condition called dysautonomia, where the autonomic nervous system, which controls heart rate, blood pressure, and digestion, stops regulating properly.
Many experience orthostatic intolerance (feeling faint on standing) and POTS (postural orthostatic tachycardia syndrome), or unstable body temperature.
Symptoms may include:
- Palpitations or rapid heart rate on sitting up.
- Dizziness or fatigue when standing in queues.
- Intolerance to heat or fluctuating room environments.
Small Fibre Neuropathy and MCAS
Small fibre neuropathy refers to damage or inflammation of the tiny nerves controlling sensation and temperature. It can manifest as burning, tingling, or sensory overload. Alongside this, Mast Cell Activation Syndrome (MCAS) can trigger flushing, rashes, histamine intolerance, and brain fog due to excessive immune cell activity.
Why Standard Long COVID Management Often Falls Short
Conventional care focuses mainly on managing symptoms by pacing, medications, and supportive therapy. While helpful for stabilisation, these methods rarely address the biological drivers like inflammation or microclots.
Importantly, graded exercise therapy can be risky for those with PEM since it can worsen rather than restore capacity.
Why Blood Filtration Is Being Explored in Long COVID
Therapeutic H.E.L.P Apheresis is a form of blood filtration used in specialised centres to remove harmful substances such as inflammatory proteins, clotting material, or abnormal lipids.
In the context of Long COVID, HELP Apheresis (Heparin-Induced Extracorporeal LDL Precipitation) is being used to:
- Reduce microclot burden.
- Remove inflammatory mediators.
- Improve microcirculation.
Learn more about the comprehensive long COVID therapy.
What HELP Apheresis Targets
The process selectively filters plasma to remove:
- Microclots.
- Inflammatory proteins.
- Excess lipoproteins that may worsen endothelial irritation.
This approach remains specialist and carefully individualised, not first-line treatment. Every patient requires a thorough assessment to ensure safety and suitability.
Apheresis Procedure
Who May (and May Not) Be a Candidate
Therapeutic apheresis may be considered for patients with:
- Persistent, multi-system Long COVID symptoms consistent with microvascular inflammation.
- Laboratory or clinical signs of endothelial dysfunction.
- Reduced quality of life despite standard therapies.
It is not suitable for those with:
- Active bleeding or clotting disorders.
- Unstable cardiovascular conditions.
- Certain medication regimens that raise the risk.
Specialist consultation is essential before determining candidacy.
What This Means for Patients Living With Long COVID
Questions to Discuss With Your Doctor
- Could persistent inflammation or microclots be contributing to my symptoms?
- What tests might help evaluate vascular or autonomic dysfunction?
- Would referral to a specialist Long COVID clinic or apheresis consultation be appropriate?
Wie wir die Ursache und nicht nur die Symptome behandeln
Unser Ansatz der Kombinationstherapie kombiniert:
- H.E.L.P. Apheresis to selectively clear spike protein, microclots, and inflammatory markers
- Inuspheresis or Immunoadsorption to remove pathogens, environmental toxins, and autoantibodies
- Nutrazeutische Mittel & Klinische Ernährungstherapie zur Unterstützung der Reparatur der Mitochondrien und des Immunsystems
- Hyperthermie (wenn angezeigt) zur Stimulierung der Immunmodulation
Erfahrungsberichte von Patienten
“I saw several doctors before coming to the Apheresis Center. They told me it was just stress. After my microclot test came back positive, I finally had proof — and a plan.”
— Robyn, UK
“Apheresis changed everything. After six sessions, my brain fog cleared and I could finally work without feeling like I’d collapse.”
— Mia, Norway
Taking the Next Step
If you’re still feeling unwell months after COVID-19, you are not alone, and you are not imagining it. Understanding the biology behind these symptoms opens new paths to recovery.
For personalised assessment or to learn more about Therapeutic Apheresis for post-COVID-19 condition, book a consultation at The Apheresis Centre today.
FAQ: Long COVID Biology and Treatment
Is Long COVID inflammatory or autoimmune?
Current peer-reviewed science tells us that Long COVID involves a combination of chronic inflammation along with immune issues, and in some patients, features of autoimmune responses rather than fitting into a single “autoimmune disease” category.
Researchers have noted persistent endothelial dysfunction along with an imbalance in cytokines and fibrin amyloid microclots, all indicating a long-lasting inflammatory state. Some groups of patients also show autoantibodies and small fiber neuropathy, which supports an autoimmune factor in a certain number of cases.
Why are my tests normal if I still feel unwell?
Standard pathology testing and imaging often focus on large-vessel issues and acute inflammation. This means it’s easy to miss microvascular changes, autonomic dysfunction, or small-fiber neuropathy on routine pathology tests. Long COVID frequently includes microscopic fibrin amyloid microclots along with endothelial dysfunction and autonomic irregularities like POTS, which standard tests do not reveal. This is why many patients are told their results are “normal” even though they continue to experience disabling symptoms.
Can vaccines reduce the risk of Long COVID?
Multiple large observational studies have shown that getting vaccinated before infection lowers the risk of developing post-COVID-19 condition, though it does not eliminate the risk. The WHO and other public health organizations emphasize that vaccination remains one of the key tools for reducing the chance and severity of Long COVID.
Author / Medical Review Note
Written by Andrew Smith. Reviewed by Dr. Inbar Tofan, Medical Director at The Apheresis Centre. Dr. Inbar has over 10 years of clinical experience in internal medicine and therapeutic apheresis, specialising in chronic inflammatory and autoimmune conditions.